Webinar Recap: “Denials Under Investigation” with Kim Conner
Kim Conner, BSN, CCDS, CCDS-O, Senior CDI Consultant/Clinical Denials Program Manager delivered a fast-paced, insight-packed session during 2025 CDI Week with her webinar, Denials Under Investigation: CDI and the Case of the Missing Documentation. Attendees walked away with practical tools to strengthen documentation, build airtight appeals, and anticipate payer tactics. The session was approved for 1 CE credit for those who attended live—yet another reason to make sure you don’t miss the next one.
“Denials are not just about coding–they’re about protecting quality, outcomes, and financial integrity.” -Kim Conner, BSN, CCDS, CCDS-O
Why Denials Can’t Be Ignored
Kim opened with a clear warning: payers are using artificial intelligence to generate denials in seconds. These denials—fair or not—still require a full response. The impact goes beyond revenue loss, extending to value-based payment models, quality scores, and patient satisfaction. In short: denials affect everything from your bottom line to your publicly reported data.
“Every automated denial still needs a thorough review–if we don’t respond, we lose that revenue.” -Kim Conner, BSN, CCDS, CCDS-O
The CDI Team as Investigators
One of the most memorable takeaways was the framing of denial management as an investigation:
- Concurrent Review Teams act as first responders, catching documentation gaps in real time.
- Second-Level Review Teams serve as forensic analysts, ensuring accuracy and consistency.
- Denial Appeals Teams step in as trial lawyers, building defensible arguments when claims are challenged.
This perspective underscores CDI’s central role in both preventing denials and protecting reimbursement when they occur.
“For CDI, we want to follow that paper trail from start to finish, making sure every clue is documented, and every case is resolved.” -Kim Conner, BSN, CCDS, CCDS-O
Red Flags and Case Studies
Payers are quick to pounce on documentation issues. Kim highlighted the most common “smoking guns”: missing evidence, inconsistent notes, and vague or templated language.
Real-world case studies brought these red flags to life:
- Sepsis cases denied because organ dysfunction wasn’t explicitly tied to sepsis.
- Respiratory failure undermined by cut-and-paste notes like “no distress.”
- Encephalopathy vs. dementia disputes that hinged on coding technicalities.
Each example showed how even the most well-documented cases can be overturned if the record leaves room for misinterpretation.
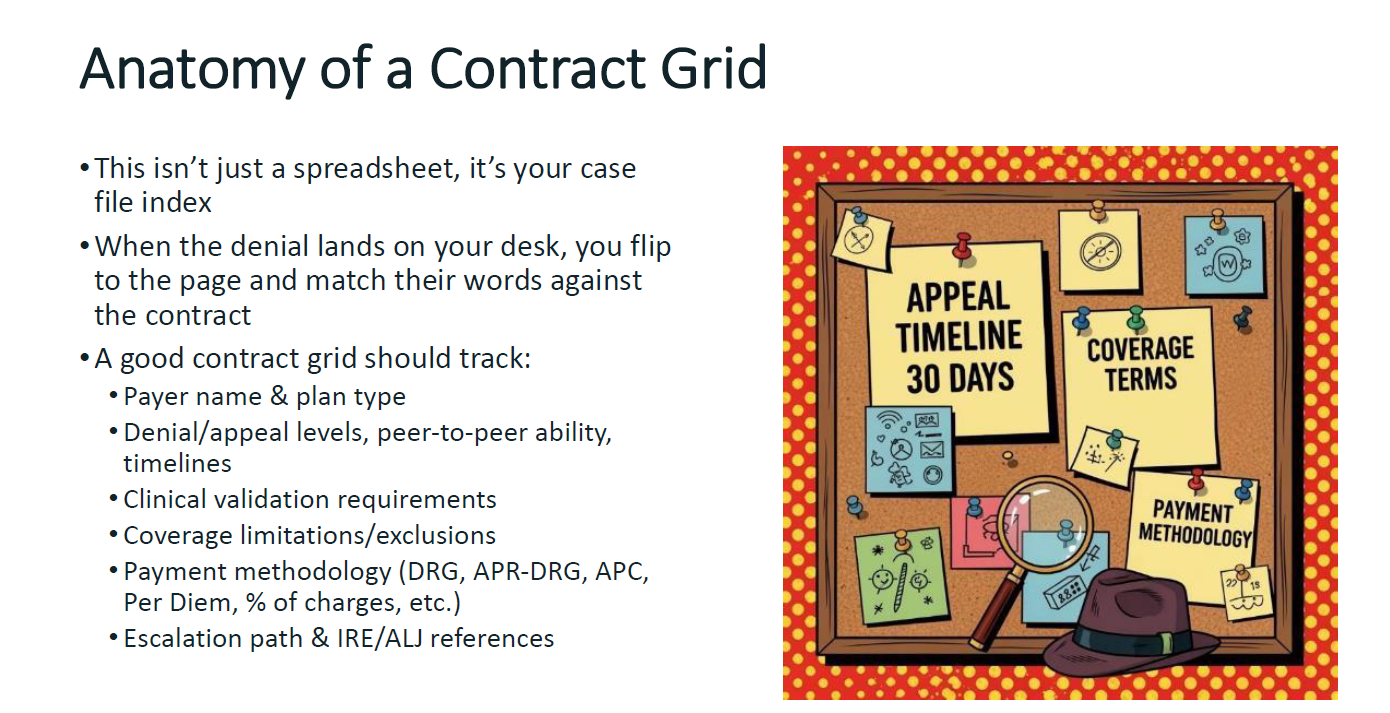
Contracts: Your Secret Weapon
Kim urged attendees to make payer contracts a core part of their appeal strategy. Audit protocols may seem authoritative, but contracts are legally binding. Her advice: build a payer contract grid that tracks requirements, timelines, and escalation paths. Being able to cite “per Section 3.5” in an appeal letter isn’t just powerful—it’s often decisive.
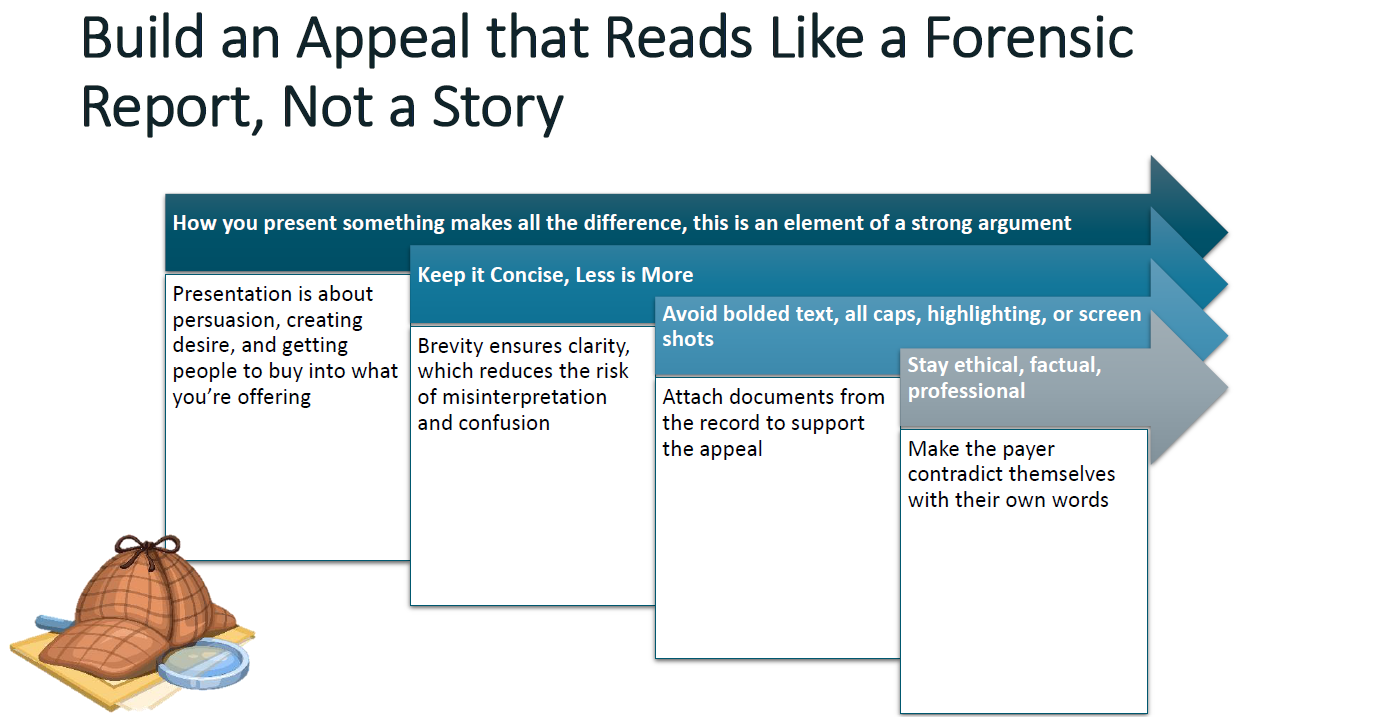
Building Better Appeals
When it comes to appeals, Kim reminded everyone that less is more. Strong letters are concise, professional, and rooted in evidence-based standards. She cautioned against emotional tone, excessive length, or formatting gimmicks. The goal: present the facts clearly, expose flawed payer tactics, and tie everything back to recognized clinical and contractual standards.
Final Word
Kim closed with a clear call to action: denial management requires vigilance, strategy, and collaboration. Strong documentation, proactive validation, and smart appeal writing aren’t optional—they’re essential.
Reminder: Only those who attended live received CE credit. Be sure to mark your calendar for the next webinar so you gain both the insights and the credit.